Common Eye Conditions
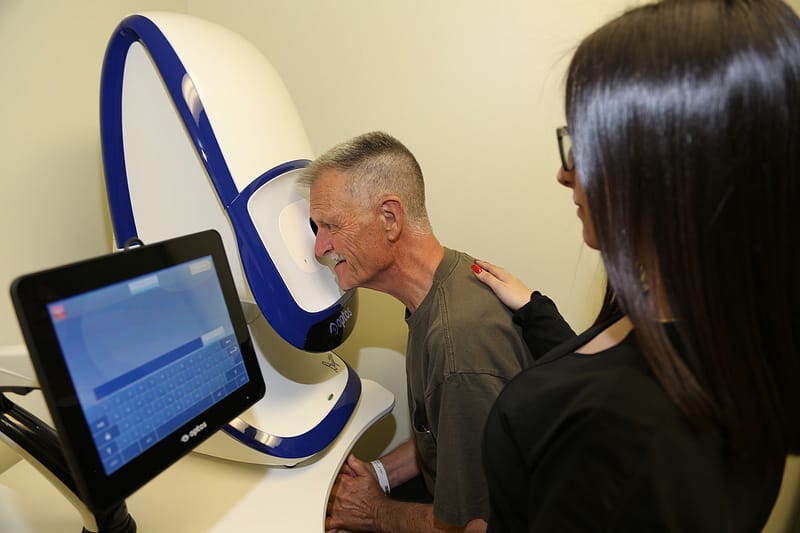
We are a comprehensive ophthalmology practice. While we specialize in cataract surgery, we diagnose and treat a variety of other common eye problems. Our experience in cataract care fosters a more personal approach to your treatment and advanced diagnostic equipment in the office allows for more extensive testing. The result is a more thorough exam. We’re a unique office with individualized care. If you have a question, let us know and we’ll respond as soon as possible during business hours.
Some more serious eye conditions can also cause redness. If you experience eye pain, a feeling that there is something in your eye (foreign body sensation), blurred vision or light sensitivity, call an eye doctor. If you wear contact lenses, you need to stop wearing them as soon as pink eye symptoms begin. If your symptoms don’t start to get better within 12 to 24 hours, make an appointment with your eye doctor to make sure you don’t have a more serious eye infection related to contact lens use.
Blepharitis is a chronic inflammation of the eyelids which causes irritation, itching and occasionally a red eye. The eyelids are composed of skin on the outside and mucous membranes on the inside. A cartilage-like plate, muscles, and glands are sandwiched in between. Blepharitis can begin in early childhood producing “granulated eyelids,” and may continue throughout life as a chronic condition or it may develop in later life. It may appear in one of two ways:
Seborrheic blepharitis is characterized by redness of the lids, scales and flaking around the eyelashes. It is often associated with dandruff of the scalp.
Ulcerative blepharitis is usually a more severe condition caused by bacteria and is characterized by matted hard crusts around the eyelashes which upon removal leave small ulcers that may bleed or ooze. The white part of the eye may turn red. In severe cases, the cornea (the clear front window of the eye) may become inflamed.
There may be a loss of eyelashes and distortion of the margins of the eyelids, which can cause chronic tearing.
Since blepharitis is a chronic condition, it is often helped by regular cleansing of the eyelids (lid hygiene). The following regimen may be useful:
- Fill a small glass with warm water.
- Add three drops of baby shampoo.
- Take a cotton wash cloth and soak it in the solution.
- Gently scrub both eyelids for two minutes with eyes closed.
- Rinse with cool tap water.
- Gently dry with a clean towel.
- Use medications as directed.
There are also commercially prepared eyelid wipes that can be used. Dr. Leonard can advise you on the best ones for your condition.
A small, red, tender bump on the inside or outside of the eyelid is most likely a stye, also called a hordeolum or chalazion. It may look like a pimple, and it can be sore. It is usually not serious and rarely affects vision.
A stye occurs when one of the glands along the eyelid becomes clogged and irritated. People usually have it on just one eyelid, but you can have one in both eyes at the same time. Some people get a stye just once, but some keep getting them.
The best treatment for a stye is warm compresses. Use a clean washcloth with very warm water over the closed eye for 5-10 minutes, several times a day. You may have to keep rewetting it as the washcloth cools. Make sure you clean off any crusting on the eyelids. Do not squeeze the stye – it could spread the infection.
Call an eye doctor if:
- it doesn’t get better in a few days
- the redness and swelling spreads beyond the eyelid, or you develop a fever
- your vision is affected
- you keep getting styes
Sharp, severe eye pain with redness, tearing, light sensitivity, and a foreign body sensation can occur when the surface of the eye is scratched. This is a common occurrence and is usually due to a corneal abrasion.
The cornea is the clear, dome-like window on the front surface of the eye; it is the structure on which contact lenses rest. The epithelium is a thin carpet like layer of cells that cover the cornea. These cells protect the deeper layers of the cornea against infection and help to provide a smooth surface to focus light onto the retina. When these cells are traumatized, the nerve endings that run in this layer are exposed, resulting in knife-like pain. This pain is similar to the pain experienced by the exposed nerve endings in a tooth cavity.
If you experience ocular trauma with pain, or if you feel that there is something in your eye that you cannot seem to get out, call Dr. Leonard or another eye care professional promptly. We will examine the eye and likely start an antibiotic drop to help prevent infection. Neglect of this problem could lead to more serious problems such as a potentially sight threatening corneal ulcer. Unfortunately, the only true cure for the pain is complete healing of the abrasion, but luckily these usually heal in 24 to 48 hours.
Since prevention is the best medicine, try to avoid corneal abrasions by wearing protective eyewear anytime you are using machinery, striking metal on metal (i.e. hammering), or working in the yard.
Glaucoma mainly occurs in adults over the age of 40, but glaucoma can sometimes affect children too. Risk factors include a family history of the disease, African-American descent, high myopia and diabetes.
Yearly examinations with Dr. Leonard will be sufficient to check for glaucoma. She will check your eye pressure, examine the optic nerve, and evaluate the drainage system in the eye.
Glaucoma is often treated with medication (eyedrops). They work by decreasing the eye pressure by either reducing fluid production in the eye or increasing outflow of fluid from the eye. Other treatment options are available including laser surgery and intraocular filtration surgery. Dr. Leonard will discuss the right treatment options for you.
Glaucoma is a chronic disease and needs to be regarded as such. It is important to keep all appointments with
Dr. Leonard and to take medications as recommended on time. Once diagnosed with glaucoma, patients need life-long care to maintain good vision. It is important to understand that glaucoma cannot be cured but it can be controlled.
Glaucoma affects an estimated 3 million Americans, with 120,000 blind due to the condition. Elsewhere in the world, glaucoma treatment is less available, and glaucoma ranks as a leading cause of blindness just about everywhere. Even if people with glaucoma do not become blind, vision can be severely impaired.
How can glaucoma be treated?
The best way to prevent vision loss from glaucoma is early diagnosis and treatment. A test called a visual field may be performed on glaucoma suspects to detect peripheral vision loss. It involves staring straight ahead into a machine and clicking a button when you notice a blinking light in your peripheral vision. The visual field test may be repeated at regular intervals to determine and monitor the extent of vision loss.
Glaucoma treatment (for any form) entails decreasing aqueous humor production, increasing fluid drainage or a combination of the two. These treatments will not restore any vision already lost to glaucoma.
There are many types of eye pressure-lowering drops including beta-blockers, alpha-2 agonists, and prostaglandin analogs. Many of the drugs used for glaucoma interact with common medications. Patients should discuss these issues with both the family physician and Dr. Leonard.
What are the different types of glaucoma?
- Open-angle glaucoma
With this most common type of glaucoma, the fluid that normally flows through the pupil into the anterior chamber of the eye cannot get through the filtration area to the drainage canals, causing a build-up of pressure in the eye. Nearly 3 million Americans – half of whom do not know they have the disease – are affected by glaucoma each year.
- Low-tension or normal-tension glaucoma
While normal intraocular pressure ranges between 12 to 21 mm Hg, an individual
may have glaucoma even if the pressure is within this range. This type of glaucoma presents optic nerve damage and narrowed side vision.
- Angle-closure glaucoma
In angle-closure glaucoma, the fluid at the front of the eye cannot reach the angle and leave the eye because the angle becomes blocked by part of the iris. This results in a sudden increase in pressure and is generally a medical emergency, requiring immediate treatment to improve the flow of fluid.
- Childhood glaucoma
Childhood glaucoma is a rare form of glaucoma that often develops in infancy, early childhood, or adolescence. Prompt medical treatment is important in preventing blindness.
- Congenital glaucoma
Congenital glaucoma, a type of childhood glaucoma, occurs in children born with defects in the angle of the eye that slow the normal drainage of fluid. Prompt medical treatment is important in preventing blindness.
- Primary glaucoma
Both open-angle and angle-closure glaucoma can be classified as primary or secondary. Primary glaucoma cannot be contributed to any known cause or risk factor.
- Secondary glaucoma
Both open-angle and angle-closure glaucoma can be classified as primary or secondary. Secondary glaucoma develops as a complication of another medical condition or injury. In rare cases, secondary glaucoma is a complication following another type of eye surgery.
What are the symptoms of glaucoma?
Most people who have glaucoma do not notice any symptoms until they begin to lose some vision. As optic nerve fibers are damaged by glaucoma, small blind spots may begin to develop, usually in the side or peripheral vision. Many people do not notice the blind spots until significant optic nerve damage has already occurred. If the entire nerve is destroyed, blindness results.
One type of glaucoma, acute angle-closure glaucoma, does produce noticeable symptoms because there is a rapid build-up of pressure in the eye. The following are the most common symptoms of this type of glaucoma. However, each individual may experience symptoms differently. Symptoms may include:
- blurred or narrowed field of vision
- severe pain in the eye(s)
- haloes (which may appear as rainbows) around lights
- redness of the eye
- nausea and vomiting
- headache
The symptoms of acute angle-closure glaucoma may resemble other eye conditions. Consult a physician immediately if you notice symptoms, as this type of glaucoma is considered a medical emergency requiring prompt medical attention to prevent blindness.
Floaters & Flashes
Flashing lights and floaters at the corner of the eye are a common occurrence for aging adults. Flashes and floaters can be benign and relatively harmless, or they can herald a significant pathological process in the back of the eye, which left unchecked can lead to loss of vision or major surgery. The only way to know if flashing light or floaters in your field of vision are benign or significant is to have Dr. Leonard dilate your eyes and examine them thoroughly.
The center of the eye is filled with a transparent gel like substance called the vitreous. As we age, the vitreous undergoes certain chemical changes. This leads to the formation of deposits of proteins which form clumps and strings floating in the gel. When light passes through the eye, the protein clumps throw a shadow on the retina producing a sensation of “floaters”.
Floaters may be seen as strings, streaks, clouds, bugs, dots, dust, or spider webs. These objects appear to be in front of the eye, but they are really floating in this fluid, and at the same time, casting their shadows on the retina, the light sensing inner layer of the eye. The debris could be made up of blood, torn retinal tissue, inflammation, vitreous detachment, or could simply mean a normal aging change in the vitreous. Floaters could also signify retinal tears that might be threatening for vision loss.
The vitreous fluid degenerates during the middle age years, often forming minute debris within the eye. Floaters are also often noticed in people who are nearsighted (myopic), and those who have been operated on for cataract or YAG laser surgery. Floaters could interfere with reading, and can be quite bothersome. Even though there is no treatment or cure, they may slowly fade out over time. One possible remedy is to move the eyes up and down when a floater appears. The vitreous fluid may shift, thus permitting the floater to move out of the line of vision.
For the most part, floaters are usually nothing to worry about, being simply a result of the normal aging development. Usually it is recommended to see an ophthalmologist within 24 hours of the onset of symptoms, as floaters could also denote a serious eye disease such as retinal detachment. The vitreous covers the retina surface, and sometimes the retina is torn when degenerating vitreous is pulled away. This leads to a small amount of bleeding, which may be interpreted as a new cluster of floaters. A torn retina is serious, and could possibly develop into a retinal detachment. Consequently, any new floaters that appear should be seen and evaluated by a doctor.
Flashes
When the vitreous gel rubs against or pulls on the retina, it can produce the illusion of flashing lights. Flashes can be perceived as a sparkle, disco light, fireflies, lightning, fireworks, Christmas tree lights or sparks. The same experience can happen after being hit in the eye, giving the illusion of seeing stars. All of these flashes are generated by any abnormal stimulus to the retina.
Light flashes can happen on and off for many weeks, or even some months. This is a common occurrence during the aging process, and it is generally not cause for concern. At times, however, a significant number of new floaters will appear, accompanied by light flashes, and partial sight loss of peripheral vision could occur. If this happens, it is important to visit your doctor quickly in order to evaluate whether the cause is a torn retina or retina detachment.
Migraine flashes appear as zigzag, shimmering, or even colorful, lines that may move within the visual field. They usually last from five to thirty minutes and can occur in both eyes at once. They are most likely caused by a sudden spasm of blood vessels in the brain. These flashes are often associated with headache, nausea, or dizziness, but more often occur without such symptoms.
As in the case with floaters, an eye specialist should attend to any abrupt onset of an abundance of light flashes. The exam would involve close observation of the retina and vitreous fluid.
Floaters and Flashes are common visual symptoms that can be representative of normal aging changes in the eye or the onset of an eye disease that could lead to vision loss if left unattended. It is always prudent to consult an eye specialist when such vision changes occur.
The retina is the light sensitive tissue at the back of the eye that acts as “the film in the camera”. It converts light into nerve signals that are transmitted along the optic nerve to the vision centers in the brain. Problems with the retina are a common cause for failing vision, especially in the elderly.
Macular Degeneration
To learn about macular degeneration, click the following links:
https://www.aao.org/eye-health/diseases/amd-macular-degeneration
https://www.aao.org/eye-health/diseases/amd-treatment
Diabetic Retinopathy
Diabetes is one of the leading causes of blindness in the United States. Leaking and bleeding blood vessels on the retina can cause severe visual loss. Effective treatments include laser photocoagulation, vitrectomy surgery and certain medications. Regular eye exams good medical management of blood sugar and blood pressure along with timely treatment can significantly reduce the risk of visual loss and blindness.
Retinal Detachment
Much like the film in a camera, the retina is responsible for creating the images one sees. When the retina detaches, it separates from the back wall of the eye and is removed from its blood supply and source of nutrition. If it remains detached, the retina will degenerate and lose its ability to function. Trauma, nearsightedness, proliferative diabetic retinopathy, and retinal tears are all possible causes of retinal detachment. Symptoms often include flashes of light, new onset of floaters, and loss of peripheral vision. If a retinal tear is discovered, detachment can usually be prevented using laser treatment. Fortunately, over 90% of retinal detachments can be repaired with a single procedure. The scleral buckle procedure, vitrectomy, and pneumatic retinopexy are three different surgical approaches for treating this condition. If you are diagnosed with retinal detachment, Dr. Leonard will discuss which option best suits you.
Sources:
“Glaucoma.”
WNY Center for the Visually Impaired, WNY Center for the Visually Impaired.
“Ulcerative Blepharitis.”
Symptoms, Diagnosis and Treatment – Symptoma®.